Did you know that 23% of the total US adult population have varicose veins? (2) Women are more affected than men. Between ages 40 and 80 years old, 22 million women and 11 million men are affected. (2)
This may seem a small number but it has greatly impacted those affected.
If you ever had questions about this common disease then this article is for you. In order to do that, we first have to understand the role veins play in our bodies.
Veins form a part of a network of vessels that carry blood back towards the heart. They are thin-walled, and distensible structures that are vital in the transport of blood and nutrients. Unlike arteries, veins carry deoxygenated blood.
Venous blood flow is different from the arterial blood flow as it is dependent on various factors such as gravity, venous valves, calf muscles, and feet pumps. (1) All these alter the venous blood flow and contribute to the dysfunctions of the veins.
Structure of Veins
Veins are specifically made for their function. Its walls are made up of three layers – intima, media, and adventitia.
The venous intima is the most inner layer of the vein walls. It is made up of an endothelial lining that produces substances that allows smooth passage of blood. (2)
Venous media refers to the middle layer of the veins. Elastic tissues and smooth muscles make up the media. (2) This functions to accommodate the expansion of the vein wall. It allows the vein to change its diameter without altering the vein pressure. (1)
The outermost layer of the vein wall is called the adventitia layer and it is most prominent in the large veins. Collagen, elastic fibers and fibroblasts compose this layer. (1) The venous adventitia gives the veins structural support and shape. (2)
Now that we understand how veins function, let’s talk about what happens in our body to cause varicose veins.
Varicose Veins and its Pathophysiology
Varicose veins are classified under the spectrum of venous insufficiency disease. Venous insufficiency is a common disease that starts as an asymptomatic cosmetic problem that further progresses into venous ulceration. (3) Varicose veins are part of the earlier gamut of chronic venous insufficiency.
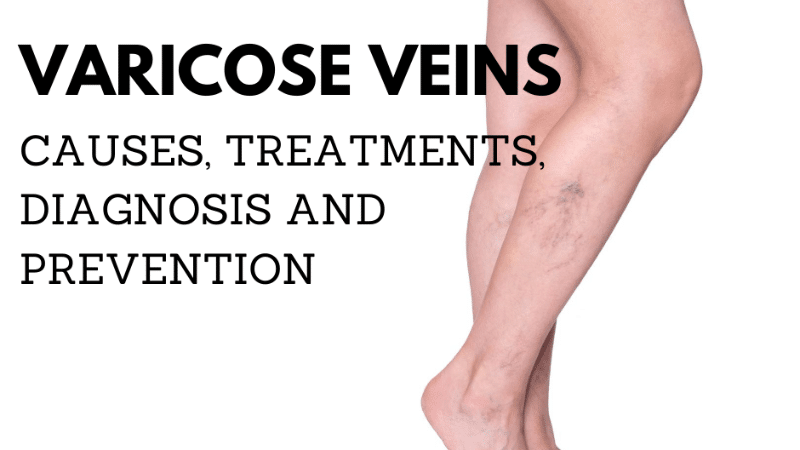
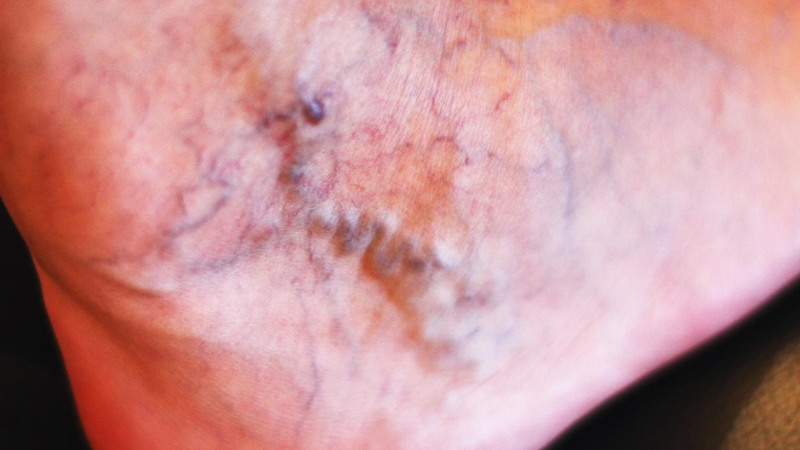
These veins are seen as tortuous vessels that protrude from beneath the skin in the lower limbs often bluish or purple in color. It has been a common problem that has caused, disability, disfigurement, and diminished quality of life.
Veins of the lower extremities are the most affected in varicose veins as they are furthest from the heart. Lower extremity veins are classified as superficial, deep, and perforating. (1) Superficial, and perforating veins are most commonly involved in varicose veins.
A variety of mechanisms causes damage to the veins but the main mechanism is the increased pressure on the veins. (4)
Increased pressure on the veins or what is termed as venous hypertension occurs when there is reflux caused by valvular incompetence, venous outflow obstruction, and calf-muscle pump failure. (5)
Competent valves make sure that blood gets to be pumped to the heart. They propel blood upward against gravity and at times, they become damaged. When there is alteration and damage to the valves, it contributes to the increased venous pressure. The changes that contribute to the valvular incompetence include stretching, splitting, tearing, thinning, and adhesion of valve leaflets. (5)
Prolonged standing or sitting also contributes to venous hypertension. This is due to the inactivity of the lower extremities and the absence of the pumping action of the muscles. Added to the weight that the lower limbs are carrying; the veins fail to pump the blood back up to the heart effectively.
The Calf-muscle pump is a force that enhances the venous blood return towards the heart. (6) In a state wherein the calf muscle is relaxed, there is an increase in venous pressure. This contributes to the reflux of blood in those with incompetent veins.
All these mechanisms affect one another resulting in varicose veins.
Risk Factors for Varicose Veins

- Hormonal
- Hormonal risk factors basically stem out from being female. Being in a high estrogen state, there is an increase in vein distensibility. (7) High levels of estrogen put women at more risk of developing varicose veins.
- Lifestyle
- Lifestyle factors that put you at more risk of developing varicose veins include occupations that involve prolonged sitting or standing such as in teachers, doctors, and nurses. As discussed earlier, prolonged standing increases the venous pressure causing reflux. (2)
- Smoking also puts you at risk of developing varicose veins. Smoking damages the wall of the veins contributing to the pathology of varicose. (8) On top of this, smoking generates highly reactive oxygen species or free radicals that could further damage and cause inflammation to the body. (8) To lessen the risk of developing varicose veins, it is best to avoid smoking.
- Acquired
- Obesity is a modifiable risk factor for varicose veins. It contributes to venous hypertension as it puts a heavyweight on lower limbs. (2) Reduction of weight is one way to prevent the progression of varicose veins. (9)
- Another acquired risk factor is pregnancy. Pregnancy is a hormonal state wherein progesterone is increased. Like estrogen, progesterone also induces venous dilation therefore it contributes to the weakened veins. (10) This increases the risk of developing varicosities. On top of this, pregnant women normally gain 11 to 16 kg of weight. (11) This adds to the venous pressure making pregnant women more at risk of developing varicose veins.
- A history of having deep vein thrombosis is also a risk factor for developing varicose veins. Deep vein thrombosis or DVT is a pathological state wherein a blood clot is formed in the deep branches of the veins. The risk of developing varicose veins is due to the post-thrombotic syndrome in DVT in the absence of primary disease. (2)
- Age is a nonmodifiable risk factor for varicose veins. (2) As we age, our bodies also undergo wear and tear. Venous valves become incompetent leading to the possibility of developing varicose veins.
- Inherited
- Varicose veins are also affected by genetics. A family history of varicose veins may put you at risk of developing it, too. Certain genes affect the vein function making it more susceptible to damage. (12)
- Other inherited diseases may also increase the risk of developing varicose veins. Ehlers-Danlos syndrome, Klippel-Trenaunay syndrome, and other gene mutations may also inherently cause varicose veins. (12)
Signs of Varicose Veins

- Blue or purple appearance of veins
- Raised veins that jut out beneath the skin
- Spider veins
Symptoms of Varicose Veins
- Heaviness of the legs
- Skin changes on the lower limbs
- Burning or throbbing of the lower legs
- Pain after prolonged sitting or standing
- Venous ulceration
- Restless Legs Syndrome
Diagnosis of Varicose Veins
History and physical examination are essential in the diagnosis of varicose veins. Physicians often examine varicose veins with the patient in a standing position. Pulses are also examined to
Imaging is also vital in the diagnosis of varicose veins. The following are the tools used in imaging:
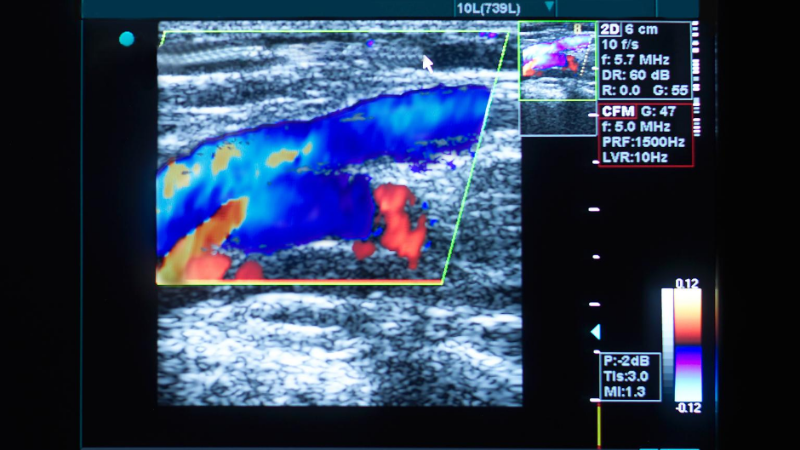
Venous duplex ultrasound scan: This is an integral tool in the diagnosis of varicose veins. It is a non-invasive, portable, and safe diagnostic tool that makes use of the sound waves and measures the speed of the blood flow. (13) It examines the vessels of the lower extremities and its accuracy is heavily dependent on the user.
Doppler ultrasonography: Similar to the ultrasound, Doppler ultrasonography is essential to the diagnosis of varicose veins or other forms of peripheral artery diseases or venous insufficiencies. (14) It is not only used in the lower extremities but also used in various parts of the body. It uses a high-frequency sound wave to measure the amount of blood flowing through your vessels. (15)
Are Varicose Veins Dangerous?
Chronic venous insufficiency is a disease where varicose veins falls under. Varicose vein is an early sign of chronic venous insufficiency. There are times where varicose veins may not be associated with chronic venous insufficiency but to be safe, patients are advised to observe their symptoms.
Progression of chronic venous insufficiency is dangerous as it may later become venous ulcerations. When left without treatment, complications may also ensue.
Bleeding is one complication of varicose veins. (16) This is especially true for superficially situated varicose veins. (17) Bleeding may seem to be harmless but bleeding varicose veins are often hard to stop. Elevation of legs and application of pressure is needed.
Varicose veins are dangerous as they could also complicate blood clot formation. This complication is called superficial thrombophlebitis. (18) This can be painful but not necessarily life-threatening.
However, superficial thrombophlebitis can progress into a deep vein clot known as deep vein thrombosis (DVT) which is dangerous and requires immediate medical attention.
Although uncommon, this could also progress into pulmonary embolism which is fatal and can cause death.
How to Prevent Varicose Veins?
While there are no ways to completely prevent varicose veins, there are supportive measures you can take to reduce your risk of getting varicose veins or developing additional ones.
The following measures to reduce the risk of varicose veins include:
- Exercise
Exercise is essential as it improves the blood flow of the lower extremities through the muscle pumping action happening in the legs. The calves function to squeeze the veins supporting the return of blood to the heart.
- Weight management
Decreasing your weight lessens the burden given to the lower extremities. This helps reduce venous hypertension.
- Eating a high-fiber, low salt diet
A vein healthy diet involves a reduction of salt intake. Increase salt intake is linked to higher blood pressure which in turn increases the risk of having hypertension and cardiovascular diseases. (19)
- Elevating your legs
Elevation of your legs decreases pressure caused by gravity and helps the blood flow back to the heart.
- Frequently changing your sitting or standing position
Changing your position also triggers the pumping action of the muscles on your legs. This helps prevent blood stasis.
Treatment for Varicose Veins
Compression Therapy
The cornerstone of varicose vein management is the use of graduated compression therapy. Graded external compression to the leg and the opposing hydrostatic forces of venous hypertension is the mechanism of compression therapy. (4) Chronic venous insufficiency is classified and graded accordingly.
Specific pressure recommendations are recommended on different classifications. For patients with varicose veins with or without edema 20 to 30 mmHg are recommended while those with advanced venous skin changes, 30 to 40 mmHg is advised. (4) For recurrent ulcers, 40 to 50 mmHg are recommended. (4)
Other treatment modalities used in treatment are the surgical approaches. There are several therapies and these are discussed below:
Radiofrequency Ablаtіоn
Radiofrequency Ablаtіоn (RFA) is a safe and minimally invasive procedure of removing varicose veins.
Unlike ligation and stripping where cuts are made over the vein, radiofrequency ablation is an endovenous treatment. This means that it is done inside the vein where thermal energy is used. It has lesser complications and high vein occlusion rates. (17)
The entire procedure can be performed on an outpatient basis. This is the preferred treatment for larger varicose veins.
Sclerotherapy
Sclerotherapy is a procedure for small and mid-sized varicose veins. It involves instilling a sclerosing solution into the veins guided by ultrasound. (17) This sclerosing agent closes up the veins. The use of graduated compression stocking is advised after this procedure.
Endovenous Thermoblation
Endovenous thermoablation is a different approach to varicose vein treatment. It is minimally invasive and it makes use of a catheter inserted to the vein involved. Using the catheter, thermal energy is delivered. This induces inflammation inside the vein and would eventually close off the vein. (17) This is an outpatient procedure making it cost-effective.
Ambulatory Phlebectomy
This procedure involves a series of small skin punctures. Localized anesthesia is given prior to the procedure. This is often done in patients with side branch varicose veins, and varicose veins of the foot, around the ankle, and the knee pit. (17)
Conclusion
Lets recap what we covered in this article one more time.
The main therapy for varicose veins is the use of graduated compression stockings. Other therapies available are also cost-effective, with minimal complications and recurrence rates.
Do you still have more questions? Are you ready to treat your varicose veins?
Book a consult today!
—
References
- Brunicardi F., Andersen D.K., Billiar T.R., Dunn D.L., Kao L.S., Hunter J.G., Matthews J.B., & Pollock R.E.(Eds.), (2019). Schwartz’s Principles of Surgery, 11e. McGraw-Hill. https://accesssurgery.mhmedical.com/content.aspx?bookid=2576§ionid=208294867
- Piazza, G. (2014). Varicose veins. Circulation: Clinical Summaries. 130(7), 582–587. https://doi.org/10.1161/CIRCULATIONAHA.113.008331
- Tucker, W.D., Arora Y., & Mahajan, K. (2020) Anatomy, Blood Vessels. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470401/
- Youn, Y. J., & Lee, J. (2019). Chronic venous insufficiency and varicose veins of the lower extremities. The Korean journal of internal medicine, 34(2), 269–283. https://doi.org/10.3904/kjim.2018.230
- Bergan JJ, Schmid-Schönbein GW, Smith PD, Nicolaides AN, Boisseau MR, Eklof B. Chronic venous disease.N Engl J Med. 2006; 355:488–498.
- Recek C. (2013). Calf pump activity influencing venous hemodynamics in the lower extremity. The International journal of angiology : official publication of the International College of Angiology, Inc, 22(1), 23–30. https://doi.org/10.1055/s-0033-1334092
- Ciardullo, A.V., et al. (2000). High endogenous estradiol is associated with increased venous distensibility and clinical evidence of varicose veins in menopausal women. Journal of vascular surgery. 32(3), 544-549. https://doi.org/10.1067/mva.2000.107768
- Gourgou, S., Dedieu, F., & Sancho-Garnier, H. (2002) Lower Limb Venous Insufficiency and Tobacco Smoking: A Case-Control Study. American Journal of Epidemiology. 155(11), 1007–1015. https://doi.org/10.1093/aje/155.11.1007
- Labropoulos, N. (2019). How Does Chronic Venous Disease Progress from the First Symptoms to the Advanced Stages? A Review. Adv Ther 36, 13–19. https://doi.org/10.1007/s12325-019-0885-3
- Mashiah, A., Berman, V., Thole, H. H., Rose, S. S., Pasik, S., Schwarz, H., & Ben-Hur, H. (1999). Estrogen and progesterone receptors in normal and varicose saphenous veins. Cardiovascular surgery (London, England), 7(3), 327–331. https://doi.org/10.1016/s0967-2109(98)00132-x
- Kominiarek, M. A., & Peaceman, A. M. (2017). Gestational weight gain. American journal of obstetrics and gynecology, 217(6), 642–651. https://doi.org/10.1016/j.ajog.2017.05.040
- Anwar, M.A., Georgiadis, K.A., Shalhoun, J., Lim, C.S., Gohel, M., & Davies, A.H. (2012). A review of familial, genetic, and congenital aspects of primary varicose vein disease. Circulation: Cardiovascular Genetics. 5(4), 460-466. https://doi.org/10.1161/CIRCGENETICS.112.963439
- Cheung M.E., & Firstenberg M.S. (2020) Duplex Ultrasound. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459266/
- Hwang J. Y. (2017). Doppler ultrasonography of the lower extremity arteries: anatomy and scanning guidelines. Ultrasonography (Seoul, Korea), 36(2), 111–119. https://doi.org/10.14366/usg.16054
- Moorthy R. S. (2002). Doppler ultrasound. Medical journal, Armed Forces India, 58(1), 1–2. https://doi.org/10.1016/S0377-1237(02)80001-6
- Tisi P. V. (2011). Varicose veins. BMJ clinical evidence, 2011, 0212.
- Campbell B. (2006). Varicose veins and their management. BMJ (Clinical research ed.), 333(7562), 287–292. https://=doi.org/10.1136/bmj.333.7562.287
- Czysz A., & Higbee S.L.(2020) Superficial Thrombophlebitis. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK556017/
- Aaron, K. J., & Sanders, P. W. (2013). Role of dietary salt and potassium intake in cardiovascular health and disease: a review of the evidence. Mayo Clinic proceedings, 88(9), 987–995. https://doi.org/10.1016/j.mayocp.2013.06.005